What is Psoriasis?
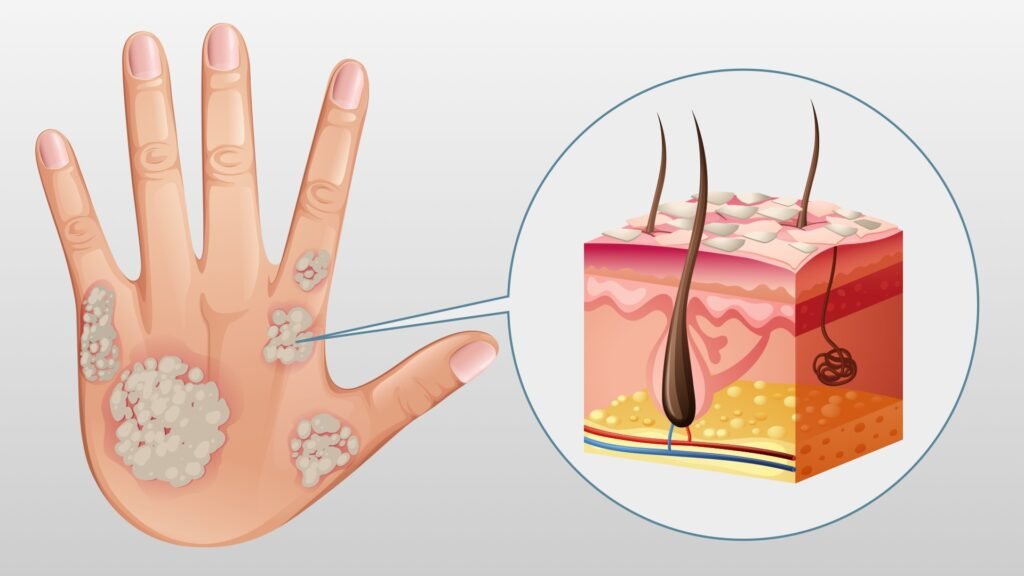
Psoriasis is a chronic, inflammatory skin condition characterized by the rapid overproduction of skin cells. This leads to the formation of red, scaly patches or plaques on the skin’s surface. It is an autoimmune disorder, meaning the body’s immune system mistakenly attacks healthy skin cells.
Psoriasis is not contagious and is typically a lifelong condition with cycles of flare-ups and remissions. The exact cause is unknown, but it is believed to be a combination of genetic and environmental factors that trigger the immune system to overreact.
There are several types of psoriasis, each with its own distinct appearance and symptoms:
-
Plaque Psoriasis: The most common form, characterized by raised, red patches covered with a silvery-white buildup of dead skin cells, often appearing on the scalp, knees, elbows, and lower back.
-
Guttate Psoriasis: Small, drop-shaped lesions that appear suddenly, often triggered by a bacterial or viral infection, commonly affecting children and young adults.
-
Inverse Psoriasis: Smooth, red lesions that occur in skin folds, such as armpits, groin, and under the breasts, often exacerbated by friction and sweating.
-
Pustular Psoriasis: Characterized by pustules (small, pus-filled blisters) surrounded by red skin, primarily affecting the hands and feet.
-
Erythrodermic Psoriasis: A rare and severe form, where widespread inflammation causes the skin to become red and shed in large sheets, often requiring hospitalization.
While psoriasis is a visible skin condition, it is more than just a cosmetic issue. It can profoundly impact an individual’s quality of life and is associated with an increased risk of other health conditions, such as psoriatic arthritis, cardiovascular disease, and depression.
Causes and Risk Factors
Psoriasis is a complex, multifactorial disease that arises from the interplay of genetic predisposition, immune system dysfunction, and environmental triggers. While the exact cause of Psoriasis is not fully understood, researchers have identified several key factors that contribute to its development and progression.
Genetic Predisposition
Psoriasis has a strong genetic component, and individuals with a family history of the disease are more likely to develop it themselves. Certain genetic variations, particularly in genes related to the immune system and skin barrier function, increase the risk of developing psoriasis. However, having these genetic predispositions does not necessarily mean an individual will develop the condition, as other factors also play a role.
Environmental Triggers
While genetics and immune system dysfunction set the stage for psoriasis, certain environmental factors can trigger or exacerbate the condition. These triggers can vary from person to person but may include:
- Stress: Psychological stress can worsen psoriasis by altering the immune system’s response and triggering inflammation.
- Infections: Certain bacterial or viral infections, such as streptococcal throat infections or HIV, can trigger or worsen psoriasis flare-ups.
- Medications: Some medications, such as lithium, antimalarials, and certain beta-blockers, can induce or exacerbate psoriasis in some individuals.
- Skin Injury: Physical trauma to the skin, including cuts, scratches, or sunburns, can cause the development of new psoriatic lesions in a phenomenon known as the Koebner phenomenon.
- Lifestyle Factors: Factors like smoking, excessive alcohol consumption, and obesity have been linked to an increased risk of developing psoriasis or worsening its symptoms.
It is important to note that these factors can interact and contribute to the development and progression of psoriasis in different ways for each individual. Understanding the underlying causes and triggers can help guide personalized treatment approaches and management strategies.
Symptoms and Signs
Psoriasis is a chronic inflammatory skin condition characterized by various visible symptoms and signs. The most prominent manifestation is the development of raised, red patches covered with silvery-white scales, known as plaques. These plaques can appear anywhere on the body, but they commonly affect the elbows, knees, scalp, and lower back.
One of the hallmark symptoms of psoriasis is the presence of skin rashes. These rashes can vary in size, shape, and severity, ranging from small, localized areas to widespread coverage across the body. The rashes often appear as raised, inflamed patches with a distinct red or pink color, and they may be accompanied by silvery-white scales that flake off easily.
Another common symptom is the formation of plaques, which are thickened, raised areas of skin covered with silvery-white scales. These plaques can be itchy, painful, and sometimes cracked or bleeding. The scales are a result of the rapid buildup of skin cells, which mature and shed at an accelerated rate in people with psoriasis.
Itching is a frequent complaint among individuals with psoriasis, and it can be intense and persistent, leading to discomfort and potential skin damage from excessive scratching. The itching is often associated with the presence of plaques and rashes, but it can also occur in areas without visible lesions.
In some cases, psoriasis can also affect the joints, leading to a condition called psoriatic arthritis. This can cause joint pain, stiffness, and swelling, particularly in the knees, ankles, fingers, and toes. Psoriatic arthritis can range from mild to severe and can significantly impact an individual’s mobility and quality of life.
It’s important to note that the severity and specific manifestations of psoriasis can vary greatly from person to person, and the symptoms may come and go in cycles, with periods of remission and flare-ups.
Diagnosis and Evaluation
Diagnosing psoriasis typically involves a combination of physical examination, medical history evaluation, and sometimes a skin biopsy. During the physical examination, a dermatologist or healthcare provider will carefully inspect the skin, looking for characteristic signs of psoriasis, such as red, raised, and scaly patches. The appearance, distribution, and pattern of these lesions can provide valuable diagnostic clues.
The medical history is also crucial in the diagnostic process. The healthcare provider will ask about the onset, duration, and progression of the symptoms, as well as any potential triggers or exacerbating factors. They may inquire about family history, as psoriasis has a genetic component, and any existing medical conditions or medications that could influence the development or manifestation of psoriasis.
In some cases, a skin biopsy may be performed to confirm the diagnosis or rule out other conditions with similar appearances. During a biopsy, a small sample of the affected skin is taken and examined under a microscope by a pathologist. The biopsy can help distinguish psoriasis from other skin disorders and identify specific subtypes of psoriasis.
Once a diagnosis of psoriasis is established, the healthcare provider will assess the severity of the condition. This assessment typically involves evaluating the extent of the affected body surface area, the location and distribution of the lesions, and the impact on the individual’s quality of life.
It’s important to note that psoriasis can sometimes be challenging to diagnose, especially in milder cases or when it presents atypically. In such situations, a multidisciplinary approach involving dermatologists, rheumatologists, or other specialists may be necessary to arrive at an accurate diagnosis and develop an appropriate treatment plan.
Treatment Options
Psoriasis is a chronic condition with no cure, but various treatment options can help manage symptoms and achieve remission. The treatment approach depends on the severity, type, and location of the psoriasis, as well as individual factors like age, overall health, and quality of life considerations.
Phototherapy
Exposing the skin to specific wavelengths of ultraviolet light can slow the rapid growth of skin cells and reduce inflammation. Common phototherapy options include:
- Narrowband UVB: This targets only the most therapeutic wavelengths of UVB light.
- Psoralen + UVA (PUVA): Psoralen, a light-sensitizing medication, is taken before UVA exposure.
- Excimer laser: This delivers a high-intensity beam of UVB light directly to the affected areas.
Systemic Medications
For moderate to severe psoriasis, oral or injectable medications that target the overactive immune system may be prescribed. These include:
- Biologics: These protein-based drugs target specific parts of the immune system.
- Traditional oral medications: Examples are methotrexate, cyclosporine, and retinoids.
Lifestyle Changes
Certain lifestyle modifications can help manage psoriasis flare-ups and improve overall well-being:
- Stress management: Techniques like meditation, yoga, and counseling can reduce stress-induced flare-ups.
- Diet: An anti-inflammatory diet rich in omega-3s may provide relief for some individuals.
- Quitting smoking: Smoking has been linked to increased severity.
- Moisturizing: Keeping the skin hydrated can reduce scaling and itching.
- Sunlight exposure: Controlled, brief sun exposure can help clear psoriasis lesions.
The most effective treatment plan often involves a combination of approaches tailored to the individual’s needs and preferences.
Living with Psoriasis
Living with psoriasis can be challenging, as the condition often has a significant impact on a person’s physical and emotional well-being. However, there are various strategies and resources available to help individuals cope with the condition and manage its effects.
Emotional Impact:
Psoriasis can have a significant emotional impact on individuals, as the visible nature of the condition can lead to feelings of self-consciousness, anxiety, and depression. It is crucial to address these emotional challenges and seek professional help if needed. Counseling or therapy can provide valuable coping mechanisms and support for managing the psychological aspects of living.
Support Resources:
These resources can provide valuable information, connect individuals with support groups, and advocate for better understanding and awareness of the condition. Some reputable organizations include the National Psoriasis Foundation, the American Academy of Dermatology, and the International Federation Associations.
Managing Flare-ups:
Developing a personalized management plan in consultation with a healthcare professional can help individuals identify and address their unique triggers, as well as implement strategies to minimize the impact of flare-ups. This may include lifestyle modifications, stress management techniques, and adhering to prescribed treatment regimens.
By adopting coping strategies, seeking support, and actively managing their condition, individuals with psoriasis can improve their overall quality of life and better navigate the challenges associated with this chronic skin condition.
Psoriasis and Comorbidities
Psoriasis is a chronic inflammatory condition that extends beyond the skin. Individuals with psoriasis are at an increased risk of developing various comorbidities, or associated conditions, which can significantly impact their overall health and quality of life.
Psoriasis can affect individuals of all ages, including the elderly population. However, managing in older adults may present unique challenges due to potential comorbidities, medication interactions, and age-related physiological changes.
In elderly individuals, psoriasis may be more difficult to treat due to thinning skin, decreased immune function, and other age-related factors.
Additionally, elderly patients with psoriasis may require additional support and assistance in managing their condition, as mobility and dexterity issues can make self-care and treatment application challenging.
Addressing psoriasis in special populations requires a tailored approach that considers the unique needs and circumstances of each individual. Close collaboration between patients, dermatologists, and other healthcare professionals is essential to ensure the best possible outcomes.
Research and Advancements
Researchers around the world are continuously working to better understand the underlying mechanisms and develop more effective treatments and potential cures. Some of the key areas of ongoing research and advancements include:
This knowledge can lead to the development of targeted therapies that address the root causes of the disease.
Immunology and Inflammation: Psoriasis is an autoimmune disorder, and researchers are investigating the role of the immune system and inflammatory processes in its pathogenesis. Understanding these mechanisms can help develop therapies that modulate the immune response and reduce inflammation.
Biologic Therapies: Biologic drugs, such as monoclonal antibodies and fusion proteins, have revolutionized the treatment.
Oral and Topical Treatments: While existing oral and topical treatments can be effective, researchers are exploring new formulations and delivery methods to improve efficacy, safety, and patient compliance.
Personalized Medicine: Researchers are exploring ways to tailor treatments based on an individual’s genetic profile, disease severity, and response to therapy. This approach aims to provide personalized and more effective treatment plans for patients.
Potential Cures: While current treatments can manage symptoms and induce remission, researchers are actively pursuing potential cures for psoriasis. This includes exploring stem cell therapies, gene editing techniques, and other cutting-edge approaches that could potentially eliminate or reverse the underlying causes of the disease.
Clinical Trials: Numerous clinical trials are underway to evaluate the safety and efficacy of new treatments, drug combinations, and therapeutic approaches. These trials are crucial for advancing our understanding and improving patient outcomes.
Overall, the research landscape is dynamic and promising, offering hope for better management, improved quality of life, and potentially curative solutions for those living with this chronic condition.
Psoriasis Awareness and Advocacy
Psoriasis is a chronic condition that can significantly impact a person’s quality of life. While research continues to advance treatment options, raising awareness and advocating for those affected by psoriasis is crucial. One of the leading organizations is the National Psoriasis Foundation (NPF), which has been at the forefront of advocacy for over 50 years. The NPF provides resources, support, and education for individuals with psoriasis and their families. They also fund research, advocate for better access to treatment, and work to raise public awareness about the condition.
Another prominent organization is the International Federation of Psoriasis Associations (IFPA), which represents associations from around the world. The IFPA aims to improve the quality of life for individuals with psoriasis by promoting advocacy, research, and education on a global scale.
Patient education is a key aspect of psoriasis awareness and advocacy efforts. Organizations like the NPF and IFPA offer educational materials, webinars, and support groups to help individuals better understand their condition, manage symptoms, and navigate treatment options. Additionally, they provide resources for healthcare professionals to improve the quality of care for patients with psoriasis.
Overall, awareness and advocacy efforts play a vital role in supporting individuals with promoting education and understanding, and driving progress in research and treatment options. By working together, organizations, healthcare professionals, and individuals affected by can continue to raise awareness, reduce stigma, and improve the overall quality of life for those living with this chronic condition.